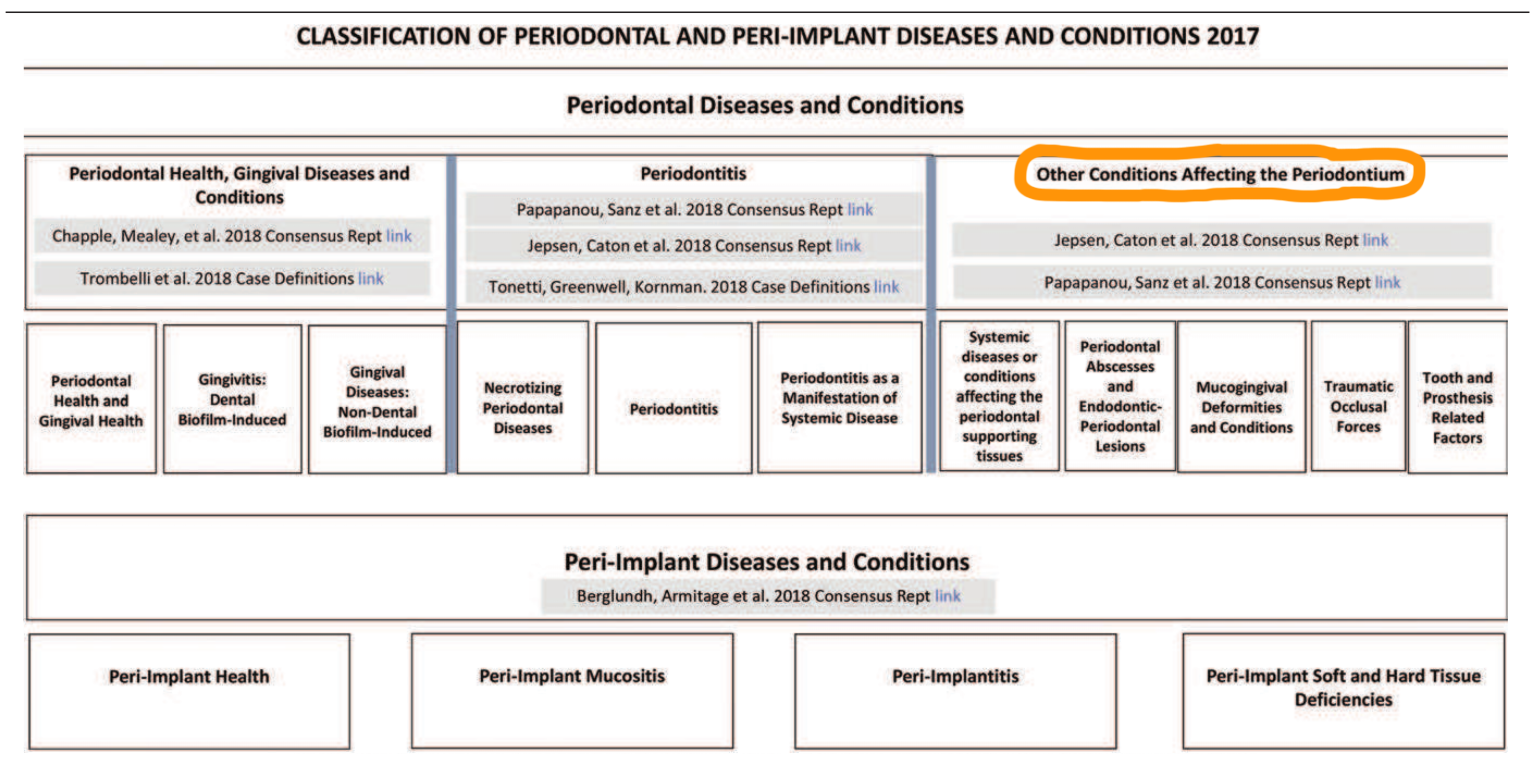
January 27, 2021
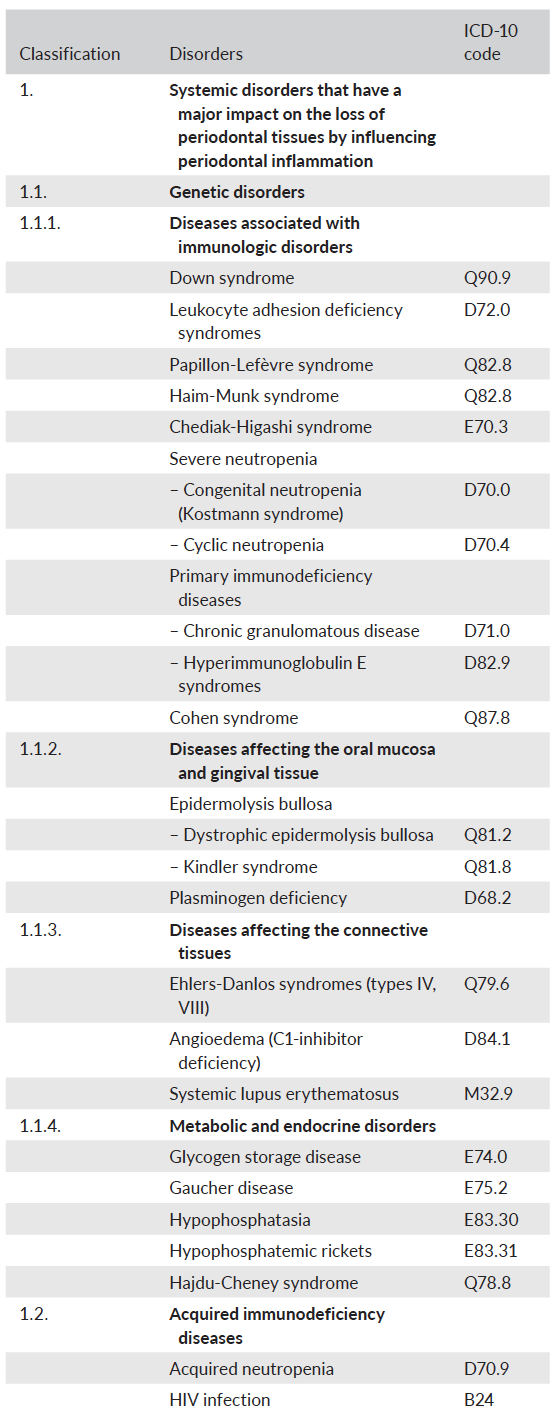
 1. How have systemic diseases and conditions that affect the periodontal supporting tissues been categorised?
1. How have systemic diseases and conditions that affect the periodontal supporting tissues been categorised?
- Under 3 major categories then subdivided
- Systemic disorders that have a major impact on the loss of periodontal tissues by influencing periodontal inflammation – genetic disorders, acquired immunodeficiency diseases, inflammatory diseases
- Other systemic disorders that influence the pathogenesis of periodontal diseases
- Systemic disorders that can result in loss of periodontal tissues independent of periodontitis – neoplasms, other disorders that may affect the periodontal tissues
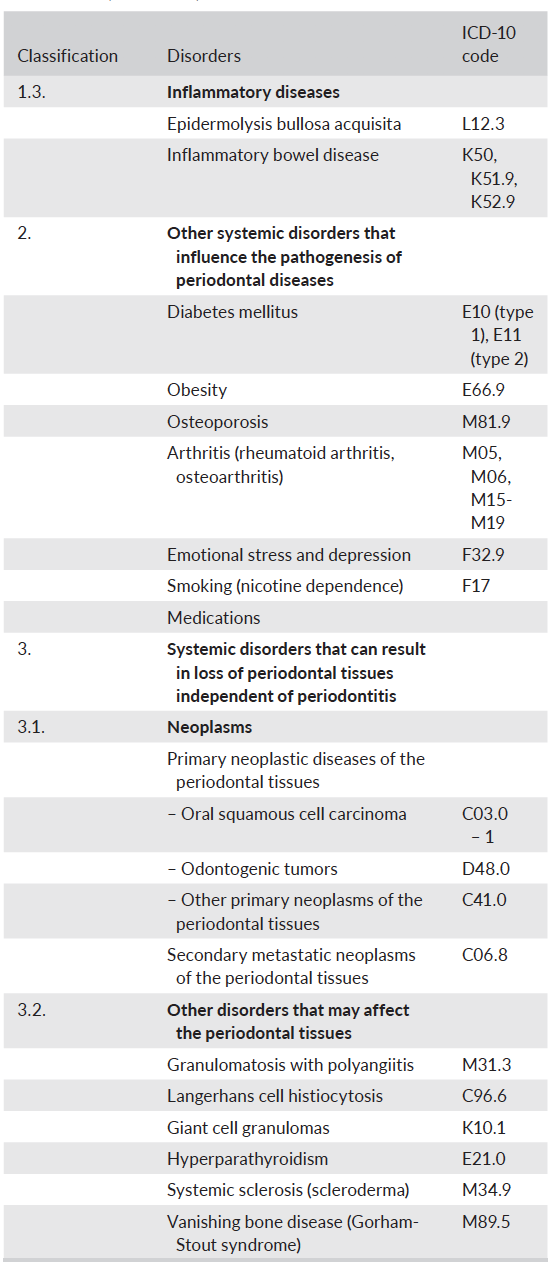 2. Why is diabetes‐associated periodontitis not a distinct diagnosis?
2. Why is diabetes‐associated periodontitis not a distinct diagnosis?
- There are no characteristic phenotypic features that are unique to periodontitis in patients with diabetes mellitus.
- Diabetes is an important modifying factor of periodontitis and should be included in a clinical diagnosis of periodontitis as a descriptor. Under the new classification of periodontitis,the level of glycaemic control in diabetes influences the grading of periodontitis.
3. Why is smoking‐associated periodontitis not a distinct diagnosis?
- Tobacco use is now considered a dependence to nicotine and a chronic relapsing medical disorder (International Classification of Diseases, Tenth Revision [ICD‐10 F17]).
- There are no unique periodontal phenotypic features of periodontitis in smokers.
- Tobacco smoking is an important modifying factor of periodontitis and should be included in a clinical diagnosis of periodontitis as a descriptor. According to the new classification of periodontitis, the current level of tobacco use influences the grading of periodontitis.
4. What does periodontal phenotype refer to, why is it relevant and how can it be measured?
- Combination of gingival phenotype (gingival thickness, keratinised tissue width) and bone morphotype (thickness of the buccal bone plate). Indicates a dimension that may change through time depending upon environmental factors and clinical intervention and can be site‐specific.
- Thin phenotype increases risk for gingival recession and are more prone to develop increasing recession lesions.
- It can be assessed by using a periodontal probe to measure the gingival thickness: Probe visible = thin (≤1 mm) and probe not visible = thick (> 1 mm). Additional information on gingival volume can be obtained by measuring the keratinised tissue width from the gingival margin to the mucogingival junction. Bone morphotypeshave been measured using CBCT but this is not recommended in this context. There is evidence reporting a correlation between gingival thickness and buccal bone plate. To date, periodontal phenotype cannot be assessed in full, while gingival phenotype can be assessed in a standardised and reproducible way.
5. What is the new classification for mucogingival conditions / recession?
- Mucogingival condition with gingival recessions – A case with gingival recession presents with an apical shift of the gingival margin. Relevant features contributing to the description of this condition are 1) the interdental clinical attachment level, 2) the gingival phenotype, 3) root surface condition, 4) detection of the CEJ, 5) tooth position, 6) aberrant frenum, and 7) number of adjacent recessions.
- Mucogingival condition without gingival recession -A case without gingival recession can be described as the gingival phenotype, either at the entire dentition, or at individual sites. Relevant features contributing to the description of this condition might be tooth position, aberrant frenum, or vestibular depth.
- Gingival recession
- Recession Type 1 (RT1): Gingival recession with no loss of interproximal attachment. Interproximal CEJ is clinically not detectable at both mesial and distal aspects of the tooth.
- Recession Type 2 (RT2): Gingival recession associated with loss of interproximal attachment. The amount of interproximal attachment loss (measured from the interproximal CEJ to the depth of the interproximal sulcus/pocket) is less than or equal to the buccal attachment loss (measured from the buccal CEJ to the apical end of the buccal sulcus/pocket).
- Recession Type 3 (RT3): Gingival recession associated with loss of interproximal attachment. The amount of interproximal attachment loss (measured from the interproximal CEJ to the apical end of the sulcus/pocket) is higher than the buccal attachment loss (measured from the buccal CEJ to the apical end of the buccal sulcus/pocket).
The table is treatment‐oriented classification approach to classify gingival phenotype, gingival recession, and associated cervical lesions.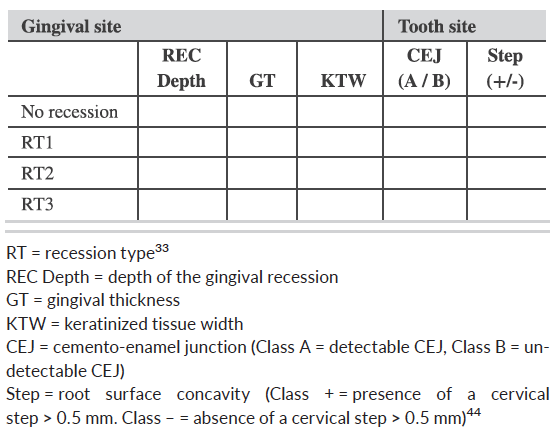 6. What are the updates on the effects of occlusion?
6. What are the updates on the effects of occlusion?
- Excessive occlusal force, now renamed to traumatic occlusal force, is defined as any occlusal force resulting in injury of the teeth and/or the periodontal attachment apparatus.Occlusal traumais a term used to describe the injury to the periodontal attachment apparatus and is a histologic term. However, a clinical diagnosis of occlusal trauma may be made in the presence of one or more of the following: progressive tooth mobility, adaptive tooth mobility (fremitus), radiographically widened periodontal ligament space, tooth migration, discomfort/pain on chewing, and root resorption.
- Primary occlusal trauma has been defined as injury resulting in tissue changes from traumatic occlusal forces applied to a tooth or teeth with normal periodontal support. This manifests itself clinically withadaptive mobility and is not progressive. Secondary occlusal trauma has been defined as injury resulting in tissue changes from normal or traumatic occlusal forces applied to a tooth or teeth with reduced support. Teeth with progressive mobility may also exhibit migration and pain on function. Current periodontal therapies are directed primarily to address aetiology; in this context, traumatic occlusal forces. Teeth with progressive mobility may require splinting for patient comfort.
- “Occlusal trauma” is in the classification and categorised as: primary occlusal trauma, secondary occlusal trauma or orthodontic forces.
 7. What is the updated term for “biologic width” and why is this relevant in the classification?
7. What is the updated term for “biologic width” and why is this relevant in the classification?
- The term biologic widthshould be replaced by supracrestal tissue attachment. The supracrestal attached tissues are histologically composed of the junctional epithelium and supracrestal connective tissue attachment.
- Infringement within the supracrestal connective tissue attachment is associated with inflammation and loss of periodontal supporting tissue. Given the available evidence, it is not possible to determine if the negative effects on the periodontium associated with restoration margins located within the supracrestal connective tissue attachment is caused by dental plaque biofilm, trauma, toxicity of dental materials, or a combination of these factors.
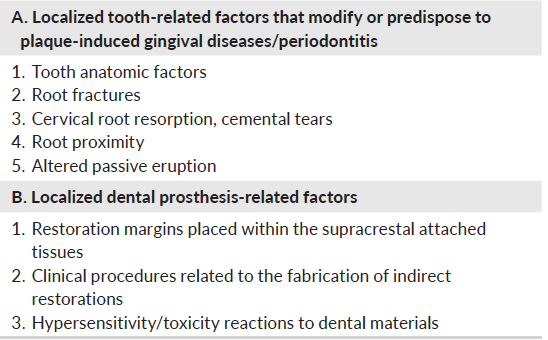
8. What do we know about the effect of dental restorations, prosthesis and other anatomical factors?
- Optimal restoration margins located within the gingival sulcus do not cause gingival inflammation if patients are compliant with self‐performed plaque control and periodic maintenance.
- The available evidence does not support that optimal fixed dental prostheses are associated with periodontitis.
- The available evidence does not support that optimal removable dental prostheses are associated with periodontitis. If plaque control is established and maintenance procedures performed, removable dental prostheses are not associated with greater plaque accumulation, periodontal loss of attachment and increased tooth mobility.
- Tooth anatomical factors (cervical enamel projections, enamel pearls, developmental grooves), root proximity, abnormalities and fractures, and tooth relationships in the dental arch are related to dental plaque biofilm‐induced gingival inflammation and loss of periodontal supporting tissues.
9. Can adverse reactions to dental materials occur?
- Dental materials may be associated with hypersensitivity reactions which can clinically appear as localised inflammation that does not respond to adequate measures of plaque control. Additional diagnostic measures are needed to confirm hypersensitivity.
10. What is altered passive eruption?
- Developmental condition with abnormal dentoalveolar relationships.
- Clinically, this condition is characterised by the gingival margin (and sometimes bone) located at a more coronal level, which leads to pseudopockets and aesthetic concerns. Correction of this condition can be accomplished with periodontal surgery.