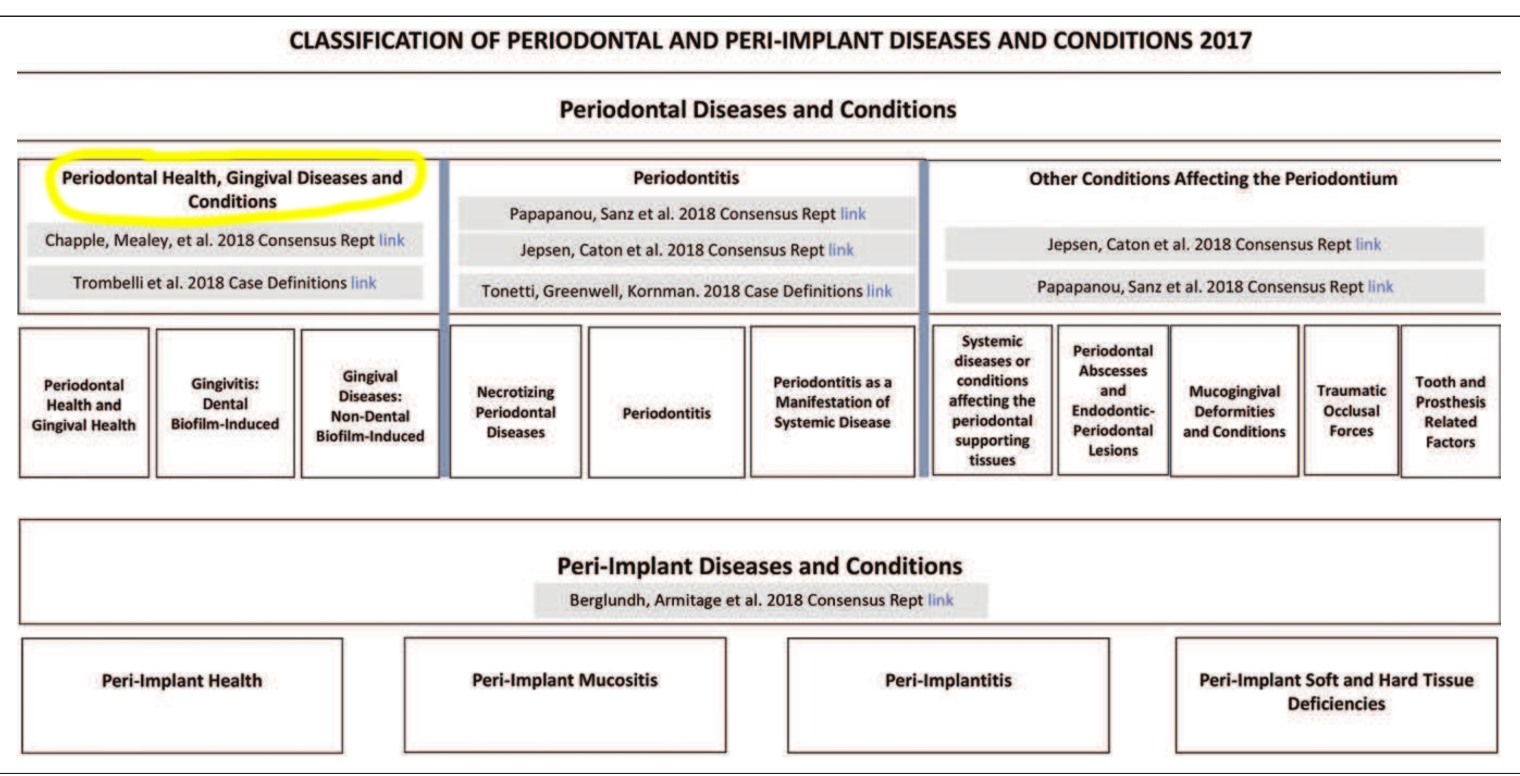
Classification of gingival health and gingival diseases/conditions
-
Why do we need a classification?
- Provides an international language for research and communication.
- Facilitates population surveys of disease prevalence.
- Enables diagnosis and prognostication for patient communication/education.
- Helps to ensure implementation of appropriate treatment.
-
Why was the 1999 classification updated?
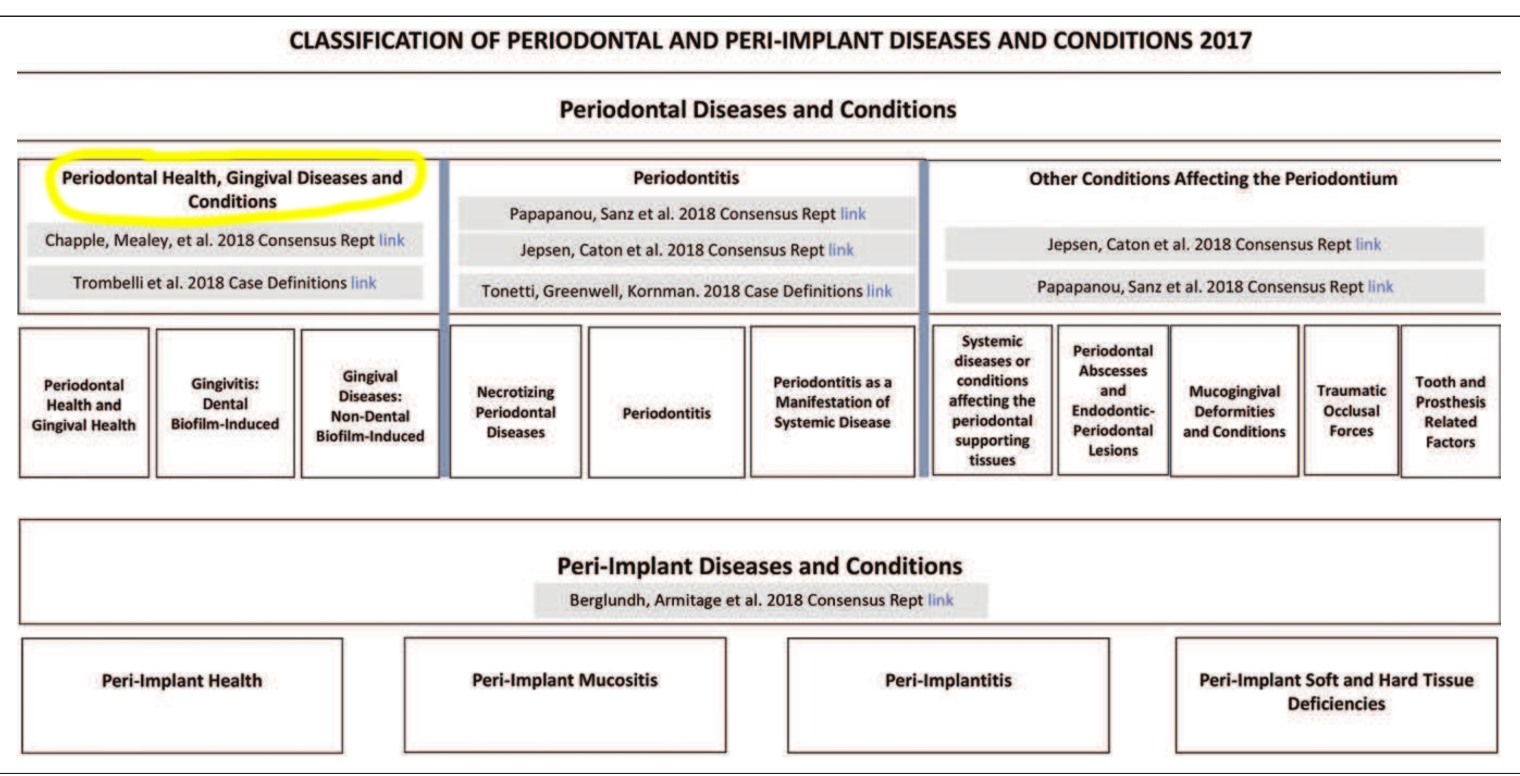
- It’s been almost 2 decades since the last comprehensive classification. The classification was updated to recognise and implicate new knowledge and understanding of current evidence.
- It aims to take a ‘precision medicine’ approach and allows oral healthcare professionals to incorporate risk factors and their management. In terms of education, it was needed to modernise curriculum content. From the public health dimension, it allows for a better understanding and management of the burden of diseases.
- The comprehensive and international assessment of current evidence provided strong basis for classifying peri-implant conditions to better guide prevention and management of peri-implant conditions at an early stage.
-
What have we learnt since the 1999 system?
- Key dynamics that may enable a “biologically-based” classification system embracing precision medicine: microbial dysbiosis, hyper-inflammatory host response, the individual patient precision medicine.
-
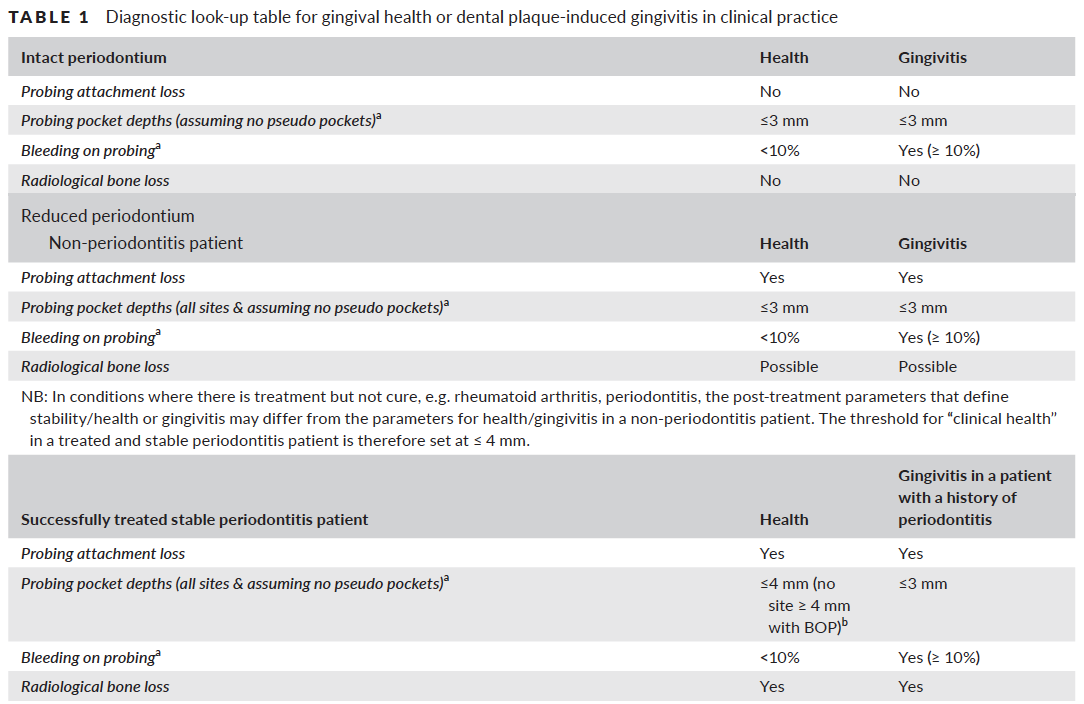
How do we classify periodontal health?
- Health is a state of complete physical, mental and social well-being and not merely an absence of disease and infirmity” – WHO 1948.
- Periodontal health is defined as the absence of clinically detectable inflammation. There is a biological level of immune surveillance consistent with gingival health and homeostasis. Pristine health is very rare.
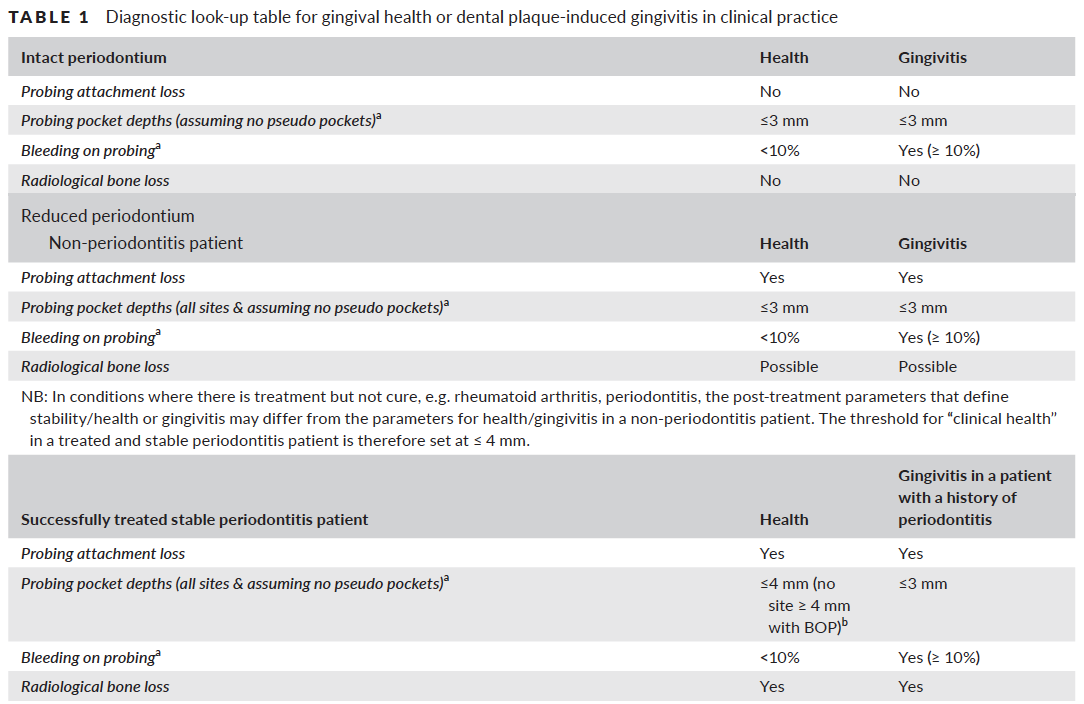
- Clinical gingival health may occur on an intact periodontium i.e. absence of detectable attachment and/or bone loss.
- Or clinical gingival health may occur on a reduced periodontium i.e. stable periodontitis patient or non-periodontitis patient (e.g. following crown lengthening).
- Clinical health can be restored following treatment of gingivitis and periodontitis.
- A “case” of clinical health presents a different situation to a “site” of clinical health.
-
Why do we need to account for a ‘reduced periodontium’ i.e. for previous periodontitis patients when diagnosing gingival health?
- It should be recognized that successfully treated and stable periodontitis patients remain at increased risk of recurrent progression of periodontitis.
- Precision medicine requires on-going individual risk assessments as part of optimal patient management and accounting for this helps with this.
-
How do you characterise gingival health of a reduced periodontium (stable periodontitis patient)?
- Periodontal stability is characterised by successful treatment through control of local and systemic risk factors, resulting in minimal (<10% of sites) BOP, no probing depths of 4 mm or greater that bleed on probing, optimal improvement in other clinical parameters and lack of progressive periodontal de
-
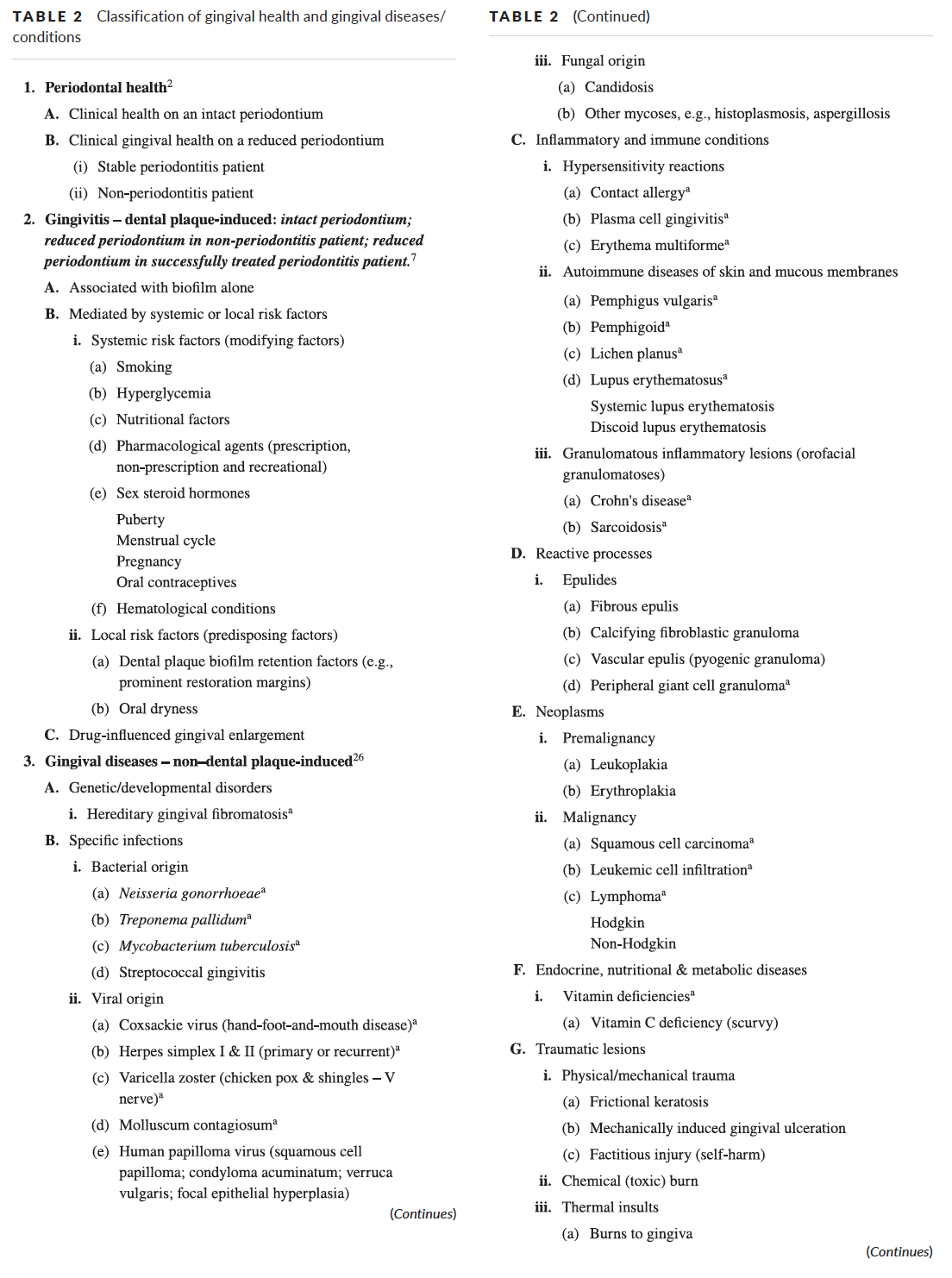
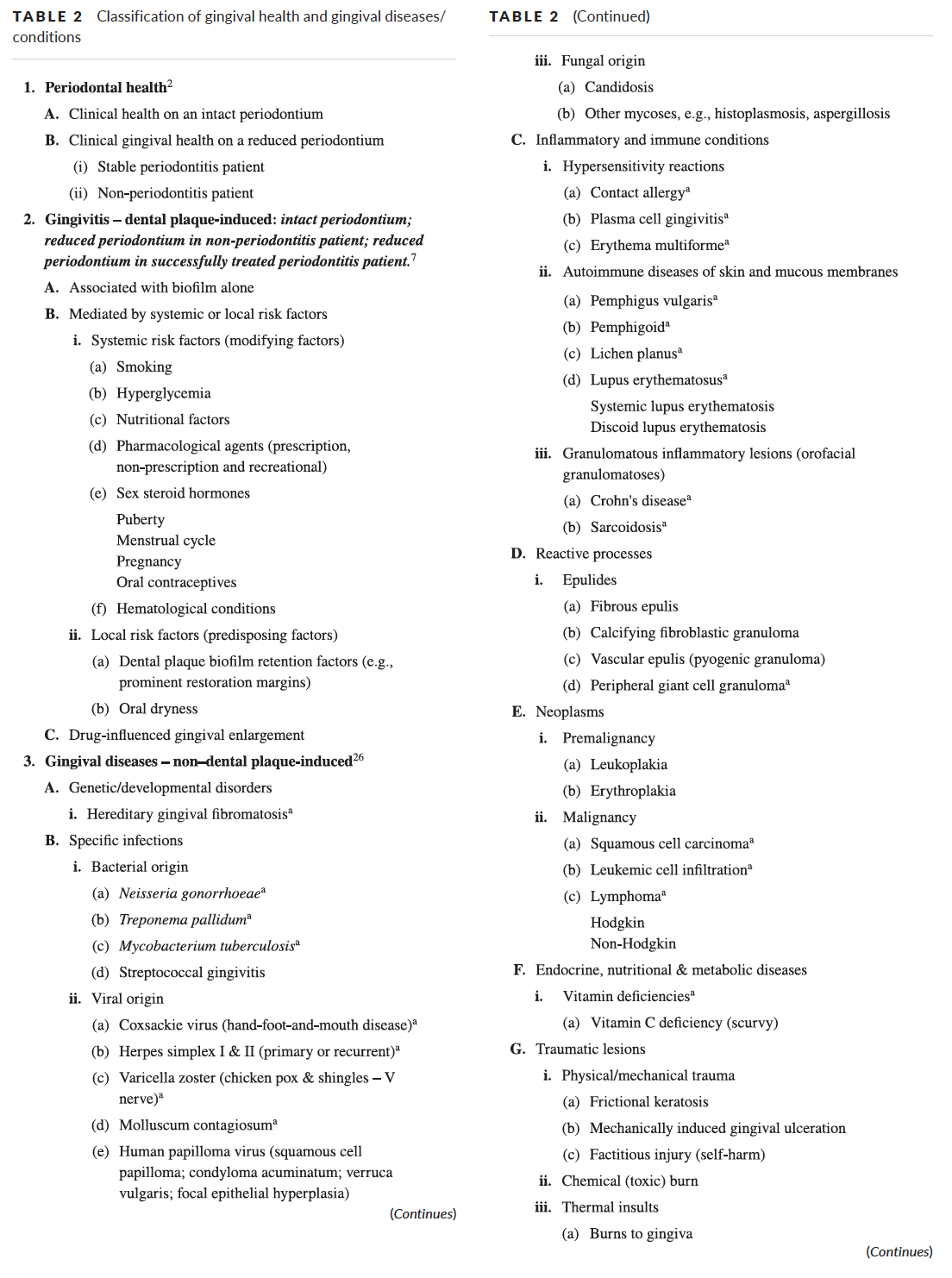
What are the categories for gingival diseases?
- Two broad categories of gingival diseases include dental plaque-induced gingivitis and non-dental plaque biofilm-induced gingival diseases.
-
How do you define dental-plaque induced gingivitis?
- At the site level: “an inflammatory lesion resulting from interactions between the dental plaque biofilm and the host’s immune-inflammatory response. Such inflammation remains confined to the gingiva and does not extend beyond the mucogingival junction and is reversible by reducing levels of dental plaque at and apical to the gingival margin”.
- Depending on whether dental plaque biofilm-induced gingival inflammation occurs on an intact or reduced periodontium, or in a patient diagnosed with periodontitis, gingivitis can be further classified as: gingivitis on an intact periodontium, gingivitis on a reduced periodontium in a non-periodontitis patient, gingival inflammation on a reduced periodontium in a successfully treated periodontitis patient.
-
How do I diagnose gingivitis?
- Assess the proportion of bleeding sites when stimulated by a standardized (dimensions and shape) periodontal probe with a controlled (∼25 N) force to the apical end of the sulcus at six sites on all teeth present.
- If there are more than or equal to 10% of sites with bleeding this is classified as gingivitis.
-
Is dental-plaque induced gingivitis a big deal?
- Yes!
- Gingivitis is a major risk factor, and a necessary pre-requisite for periodontitis. The management of gingivitis is thus a primary prevention strategy for periodontitis.
-
When diagnosing plaque-induced gingivitis you can also subclassify it to take into account local risk factors/predisposing factors and systemic risk factors/modifying factors. What would this include?
- Local risk factors (predisposing factors) include dental plaque-biofilm retention factors (e.g. tooth anatomy, restorative margins) and oral dryness (reduction in salivary flow or quality due to medications, mouth breathing or Sjögren’s).
- Systemic risk factors (modifying factors) include smoking, metabolic factors, nutritional factors, pharmacological agents, elevations in sex steroid hormones and haematological conditions.
-
How do we classify non–dental plaque‐induced gingival conditions?
- Non-dental plaque biofilm-induced gingival diseases include a variety of conditions that are not caused by plaque and usually do not resolve following plaque removal. Such lesions may be manifestations of a systemic condition or may be localised to the oral cavity.
- To help distinguish this from inflammation induced by biofilm, a clue would be that if the inflammation extends beyond the mucogingival junction then this is unlikely to be biofilm-induced.
- These are categorised under: genetic/developmental; specific infections; inflammatory and immune conditions; reactive processes; neoplasms; endocrine, nutritional and metabolic disorders; traumatic lesions and gingival pigmentation.
- Some of these have associated systemic involvement or are oral manifestations of systemic conditions so other health-care providers may be involved in diagnosis and treatment.
Periodontology
Recent post
June 29, 2023
Pink Aesthetics...
Read more
General Dental,Periodontology
June 26, 2022
10 Key Points from EuroPerio10...
Read more
Periodontology,Reena's Notes
June 11, 2021
Working as a hygienist or therapist...
Read more
General Dental,Periodontology